


中华护理杂志 ›› 2026, Vol. 61 ›› Issue (2): 190-197.DOI: 10.3761/j.issn.0254-1769.2026.02.006
李昉1( ), 徐翠荣2,*(
), 徐翠荣2,*( ), 姜琳1, 张李霞1, 肖艳华1, 原晓1, 黄朝阳1, 包佳威3
), 姜琳1, 张李霞1, 肖艳华1, 原晓1, 黄朝阳1, 包佳威3
收稿日期:2025-04-22
出版日期:2026-01-20
发布日期:2026-01-14
*通讯作者:
徐翠荣,E-mail:xucuirong67@163.com作者简介:李昉:女,本科,主管护师,E-mail:493122906@qq.com
基金资助:
LI Fang1( ), XU Cuirong2,*(
), XU Cuirong2,*( ), JIANG Lin1, ZHANG Lixia1, XIAO Yanhua1, YUAN Xiao1, HUANG Chaoyang1, BAO Jiawei3
), JIANG Lin1, ZHANG Lixia1, XIAO Yanhua1, YUAN Xiao1, HUANG Chaoyang1, BAO Jiawei3
Received:2025-04-22
Online:2026-01-20
Published:2026-01-14
* Corresponding author:
XU Cuirong,E-mail:xucuirong67@163.comFunding program:摘要:
目的 分析早产儿经下肢置入PICC并发静脉炎的影响因素,构建并验证风险预测模型,为早期识别及预防静脉炎提供参考。方法 采用便利抽样法,选取2019年1月—2022年12月在南京市某三级甲等综合医院行下肢PICC置管的366例早产儿作为建模组,选取2023年1月—2024年12月行下肢PICC置管的158例早产儿作为验证组,回顾性收集相关资料,采用Logistic回归分析探究早产儿经下肢置入PICC并发静脉炎的影响因素,构建风险预测模型,并评价其预测效果。结果 在建模组中有97例发生了静脉炎,发生率为26.50%。Logistic回归分析结果显示,胎龄、是否输注刺激性药物、穿刺静脉、穿刺部位、穿刺总时长、穿刺后7 d内更换敷料的次数是早产儿经下肢置入PICC并发静脉炎的影响因素(P<0.05)。依据以上结果构建风险预测模型,验证组中,模型的最佳截断值为0.311,准确率为92%,灵敏度为94%,特异度为88%,阳性预测值为0.94,阴性预测值为0.86;Hosmer-Lemeshow检验结果显示,χ2=8.100(P=0.424)。结论 早产儿经下肢置入PICC并发静脉炎风险预测模型具有良好的区分度、校准度,可为新生儿科护士预测相关风险提供参考。
李昉, 徐翠荣, 姜琳, 张李霞, 肖艳华, 原晓, 黄朝阳, 包佳威. 早产儿经下肢置入PICC并发静脉炎风险预测模型的构建与验证[J]. 中华护理杂志, 2026, 61(2): 190-197.
LI Fang, XU Cuirong, JIANG Lin, ZHANG Lixia, XIAO Yanhua, YUAN Xiao, HUANG Chaoyang, BAO Jiawei. Construction and verification of a risk prediction model for venous inflammation in preterm neonates with PICC placed in lower limbs[J]. Chinese Journal of Nursing, 2026, 61(2): 190-197.
 |
表1 调查对象的一般资料及经下肢置入PICC并发静脉炎影响因素的单因素分析结果
Table 1 General information of the survey subjects and the results of univariate analysis of phlebitis complicated by PICC inserted via the lower limbs
 |
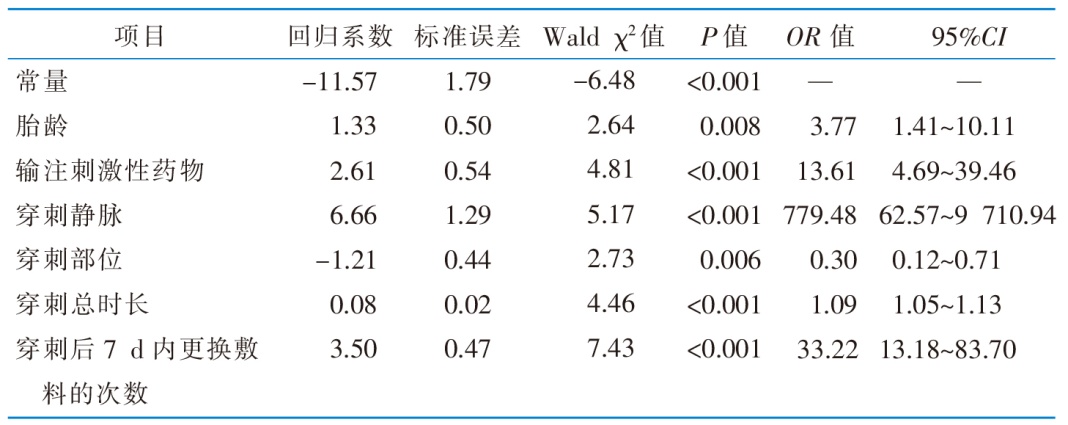 |
表2 早产儿经下肢置入PICC并发静脉炎影响因素的Logistic回归分析结果(n=366)
Table 2 Results of Logistic regression analysis on risk factors for phlebitis complicated by PICC inserted via lower limbs in preterm infants(n=366)
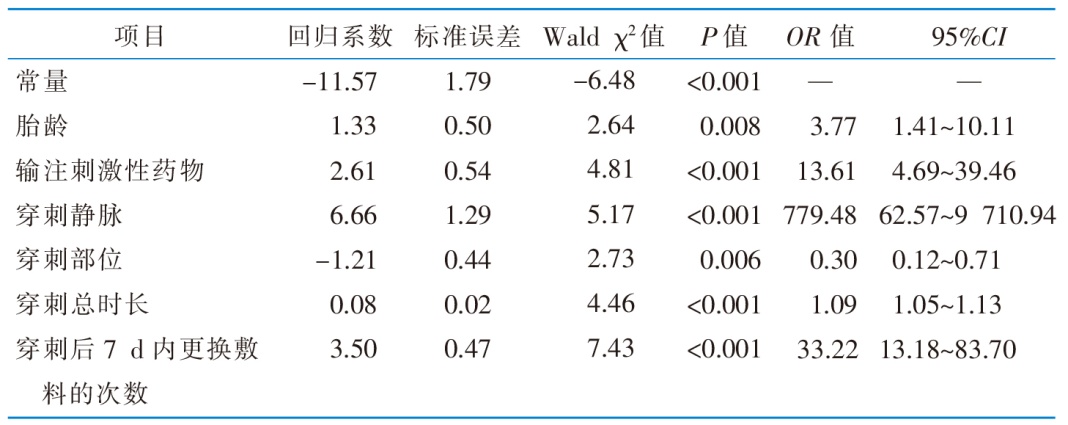 |
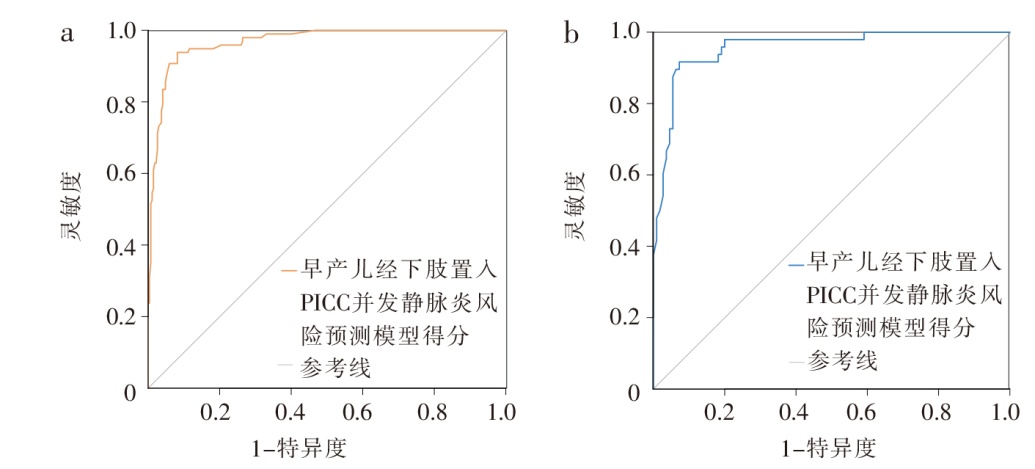
图2 早产儿经下肢置入PICC并发静脉炎风险预测模型的受试者操作特征曲线
Figure 2 Receiver operating charac-teristic curve of the prediction model for phlebitis following lower limb PICC insertion in preterm infants
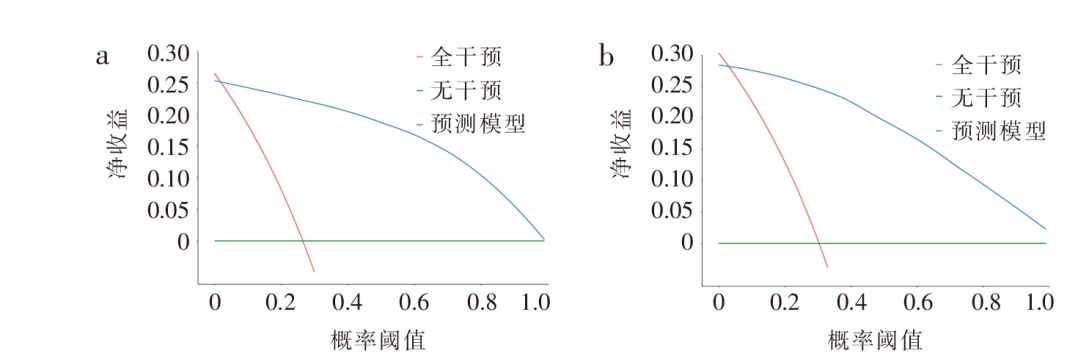
图3 早产儿经下肢置入PICC并发静脉炎风险预测模型的决策曲线 注:a为建模组,b为验证组。
Figure 3 Decision curve analysis of the prediction model for phlebitis following lower limb PICC insertion in preterm infants
| [1] | 凌其英, 魏娇, 万舸, 等. 心电监护仪在新生儿经下肢静脉置入中心静脉导管中定位效果的随机对照研究[J]. 中国当代儿科杂志, 2022, 24(10):1124-1129. |
| Ling QY, Wei J, Wan G, et al. Efficiency of electrocardiogram monitor for positioning the catheter tip in the central catheter placement via lower extremity veins in neonates:a randomized controlled study[J]. Chin J Contemp Pediatr, 2022, 24(10):1124-1129. | |
| [2] |
Nickel B, Gorski L, Kleidon T, et al. Infusion therapy standards of practice,9th edition[J]. J Infus Nurs, 2024, 47(Suppl 1):S1-S285.
DOI URL |
| [3] | 谢巧庆, 何春梅, 黄科志, 等. 新生儿PICC置入后并发机械性静脉炎风险预测模型的构建及验证[J]. 循证护理, 2025, 11(4):699-703. |
| Xie QQ, He CM, Huang KZ, et al. Construction and verification of a risk prediction model of mechanical phlebitis after PICC implantation[J]. Chin Evid Based Nurs, 2025, 11(4):699-703. | |
| [4] | 杨丽娟, 徐兵, 戴明红, 等. 危险因素评估下针对性护理干预对新生儿PICC静脉炎预防效果分析[J]. 蚌埠医学院学报, 2023, 48(9):1278-1281. |
| Yang LJ, Xu B, Dai MH, et al. Effect of targeted nursing inter-ventions on PICC-associated phlebitis prevention in neonates under risk factor assessment[J]. J Bengbu Med Coll, 2023, 48(9):1278-1281. | |
| [5] | 杨丽娟, 刘丽华, 伏蕤, 等. PICC置入病人并发机械性静脉炎列线图预测模型的构建[J]. 护理研究, 2021, 35(10):1746-1750. |
| Yang LJ, Liu LH, Fu R, et al. Construction of a nomogram prediction model for patients with PICC placement complica-ted with mechanical phlebitis[J]. Chin Nurs Res, 2021, 35(10):1746-1750. | |
| [6] |
沈婷, 余婷, 聂玲, 等. 新生儿PICC导管尖端继发性异位预防和处理的最佳证据总结[J]. 中华护理杂志, 2023, 58(18):2273-2281.
DOI |
|
Shen T, Yu T, Nie L, et al. Summary of the best evidence for the prevention and management of PICC secondary catheter tip malposition in neonates[J]. Chin J Nurs, 2023, 58(18):2273-2281.
DOI |
|
| [7] |
韩姗姗, 秦永平, 屈虹, 等. 神经外科患儿术中获得性压力性损伤风险预测模型的构建及验证[J]. 中华护理杂志, 2025, 60(8):928-933.
DOI |
|
Han SS, Qin YP, Qu H, et al. Construction and validation of a risk prediction model for intraoperative acquired pressure injury in neurosurgical children[J]. Chin J Nurs, 2025, 60(8):928-933.
DOI |
|
| [8] | 孙兴, 徐微, 刘蓓蓓, 等. 极低/超低出生体质量儿经外周静脉穿刺中心静脉置管过程中发生机械性静脉炎的影响因素分析[J]. 实用临床医药杂志, 2023, 27(23):110-114. |
| Sun X, Xu W, Liu BB, et al. Influencing factors of mechanical phlebitis in very/extremely low birth weight infants with peri-pherally inserted central catheterization[J]. J Clin Med Pract, 2023, 27(23):110-114. | |
| [9] |
韩林, 李敏敏, 李雨欣, 等. 先天性心脏病术后患儿营养不良风险预测模型的构建及验证研究[J]. 中华护理杂志, 2024, 59(19):2396-2403.
DOI |
|
Han L, Li MM, Li YX, et al. Construction and verification of a risk prediction model for postoperative malnutrition in infants with congenital heart disease[J]. Chin J Nurs, 2024, 59(19):2396-2403.
DOI |
|
| [10] | 张玉侠. 实用新生儿护理学[M]. 北京: 人民卫生出版社, 2015:629-631. |
| Zhang YX. Practice of neonatal nursing care[M]. Beijing: People’s Medical Publishing House, 2015:629-631. | |
| [11] |
Gorski LA. Update:the 2024 infusion therapy standards of pra-ctice[J]. Home Healthc Now, 2024, 42(4):198-205.
DOI PMID |
| [12] | 张月葵, 郭舒文, 杨玉燕, 等. 新生儿经右下肢小隐静脉留置PICC导管的效果研究[J]. 护理研究, 2023, 37(3):543-547. |
| Zhang YK, Guo SW, Yang YY, et al. Study on the effect of PICC catheter indentation through small saphenous vein of right lower limb in neonates[J]. Chin Nurs Res, 2023, 37(3):543-547. | |
| [13] |
沈巧, 唐语蔓, 冷虹瑶, 等. 新生儿疼痛评估量表测量学性能的系统评价再评价[J]. 中国全科医学, 2022, 25(35):4453-4461.
DOI |
| Shen Q, Tang YM, Leng HY, et al. Psychometric properties of the Pain Assessment Scales in Newborns:an overview of sys-tematic review[J]. Chin Gen Pract, 2022, 25(35):4453-4461. | |
| [14] | 陈琼, 李颖馨, 胡艳玲, 等. 新生儿经外周置入中心静脉导管操作及管理指南(2021)[J]. 中国当代儿科杂志, 2021, 23(3):201-212. |
| Chen Q, Li YX, Hu YL, et al. Operation and management guidelines for peripherally inserted central catheter in neona-tes(2021)[J]. Chin J Contemp Pediatr, 2021, 23(3):201-212. | |
| [15] | 李蕊, 王晶, 王佳琦, 等. 极/超低出生体质量儿经外周静脉置入中心静脉导管相关并发症及影响因素分析[J]. 解放军护理杂志, 2020, 37(4):51-54. |
| Li R, Wang J, Wang JQ, et al. Analysis of PICC-related complications and related factors in very/extremely low birth weight infants[J]. Nurs J Chin PLA, 2020, 37(4):51-54. | |
| [16] | 李智英, 司徒妙琼, 吕林华. 低出生体质量儿PICC置管后导管相关并发症的相关因素分析[J]. 重庆医学, 2017, 46(34):4886-4888. |
| Li ZY, Situ MQ, Lü LH. Analysis of related factors of ca-theter-related complications after PICC catheterization in low birth weight infants[J]. Chongqing Med, 2017, 46(34):4886-4888. | |
| [17] |
Wu YH, Yan J, Tang MY, et al. A review of neonatal periphe-rally inserted central venous catheters in extremely or very low birthweight infants based on a 3-year clinical practice:Complication incidences and risk factors[J]. Front Pediatr, 2022, 10:987512.
DOI URL |
| [18] | 漆永林, 王芳, 匡湘娟, 等. 温度干预对早产儿PICC置管疼痛及置管效果的影响[J]. 昆明医科大学学报, 2025, 46(1):167-172. |
| Qi YL, Wang F, Kuang XJ, et al. Impact of temperature inter-vention on pain and catheterization outcomes in premature infants undergoing PICC placement[J]. J Kunming Med Univ, 2025, 46(1):167-172. | |
| [19] |
Guven H. Fluid dynamics and venous hemodynamics in the lower extremities[J]. Vasa, 2024, 53(5):308-313.
DOI PMID |
| [20] |
Chen XW, Lin C, Yue LQ, et al. Placement of peripherally in-serted central catheters in neonates:a retrospective study[J]. Nurs Crit Care, 2024, 29(6):1680-1686.
DOI URL |
| [21] |
林楠, 诸纪华, 徐红贞, 等. 早产儿体位管理的最佳证据总结[J]. 中华护理杂志, 2022, 57(4):486-492.
DOI |
| Lin N, Zhu JH, Xu HZ, et al. Best evidence summary of posi-tioning management for preterm infants[J]. Chin J Nurs, 2022, 57(4):486-492. | |
| [22] | 唐云飞, 赵菲菲, 居佳. 水胶体透明敷料预防新生儿葡萄糖酸钙静脉炎的效果研究[J]. 解放军护理杂志, 2018, 35(20):74-76. |
| Tang YF, Zhao FF, Ju J. Effect of hydrocolloid transparent dressing on prevention of neonatal phlebitis induced by calcium gluconate[J]. Nurs J Chin PLA, 2018, 35(20):74-76. | |
| [23] | 陈玉. 以问题为中心的持续质量改进在预防新生儿PICC置管术后机械性静脉炎中的应用[J]. 护理实践与研究, 2019, 16(14):152-154. |
| Chen Y. Application of problem-centered continuous quality improvement in the prevention of neonatal mechanical phle-bitis after PICC catheterization[J]. Nurs Pract Res, 2019, 16(14):152-154. | |
| [24] | 章容, 刘兴琴, 刘晓玲, 等. 早产儿经外周中心静脉置管时加温皮肤消毒剂对置管效果的影响[J]. 中华新生儿科杂志, 2022, 37(3):254-257. |
| Zhang R, Liu XQ, Liu XL, et al. Effect of warmed skin disinfectant on catheterization outcomes during peripherally inserted central catheter placement in preterm infants[J]. Chin J Neonatol, 2022, 37(3):254-257. | |
| [25] | 高锦华, 吴佳音, 邓素芬, 等. 早产儿经外周中心静脉置管敷料更换频率安全性的随机对照研究[J]. 中华新生儿科杂志, 2021, 36(6):33-37. |
| Gao JH, Wu JY, Deng SF, et al. Randomized controlled trial on the safety of dressing change frequency for peripherally inserted central catheters in preterm infants[J]. Chin J Neona-tol, 2021, 36(6):33-37. |
| [1] | 祝海香, 李艳, 许启锦, 陈瑾萱, 韩小雪, 吴缘. 慢性心力衰竭患者分级分类症状识别工具的研制及应用研究[J]. 中华护理杂志, 2026, 61(2): 149-156. |
| [2] | 王蔚云, 顾则娟, 汤一帆, 苏子雯, 刘长红. 心力衰竭患者的液体平衡阈值研究及护理对策[J]. 中华护理杂志, 2026, 61(2): 157-165. |
| [3] | 吴晓敏, 谷艳荣, 柴依依, 马心蕊, 朱豆, 张政, 林平, 李玲. 急性心肌梗死介入术后患者恐惧体验及应对需求的质性研究[J]. 中华护理杂志, 2026, 61(2): 166-173. |
| [4] | 章盈盈, 马燕, 吴黎莉, 张丽, 孙莹, 刘璐, 庄一渝. 心血管疾病患者症状感知困境量表的编制及信效度检验[J]. 中华护理杂志, 2026, 61(2): 174-181. |
| [5] | 陶娟, 尹永田, 秦玉婷, 王诗源, 韩榕, 张瀚丹. 左心室辅助装置植入患者照顾者居家照护体验的Meta整合[J]. 中华护理杂志, 2026, 61(2): 182-189. |
| [6] | 曾晗月, 彭寅森, 陈腾霞, 李韵, 朱守淋, 黄乐娇, 王彩莲, 毛世芳. 《成人有创机械通气气道内吸引技术操作》团体标准临床实践现状及影响因素分析[J]. 中华护理杂志, 2026, 61(2): 198-204. |
| [7] | 丁佳蓉, 陈慧, 王雪瑞, 孙小玲, 张银. 原位新膀胱术后尿失禁患者自我管理体验及需求的纵向质性研究[J]. 中华护理杂志, 2026, 61(2): 205-212. |
| [8] | 杜雪莲, 陈华健, 黄少娟, 李灿辉, 董佩文, 廖江波, 区博伟. 骨盆骨折患者风险评估系统的开发与应用研究[J]. 中华护理杂志, 2026, 61(2): 213-219. |
| [9] | 李雪梅, 李永琦, 刘颖, 李俊英, 时瑾瑾, 张兰, 江会. 母婴分离产妇母乳喂养集束化护理干预方案的构建及应用研究[J]. 中华护理杂志, 2026, 61(2): 220-228. |
| [10] | 吴萍, 于宛辰, 柳嘉怡, 尹思文, 王汕珊. 养老护理员死亡认知及应对能力的潜在剖面分析[J]. 中华护理杂志, 2026, 61(2): 229-236. |
| [11] | 兰星, 刘婷, 李勍, 柯稳, 李鑫, 张转运, 翟洁, 刘佳佳. 700所医疗机构麻醉科专科护士工作及管理现状的调查研究[J]. 中华护理杂志, 2026, 61(2): 237-243. |
| [12] | 周帅帅, 王飒, 刘亚洁, 柴晶晶, 闫丹萍, 王钰炜. 1例胃内镜黏膜下剥离术后迟发性出血并发腹腔间隔室综合征患者的急救护理[J]. 中华护理杂志, 2026, 61(2): 244-248. |
| [13] | 蒋伟红, 唐晓敏, 周军, 朱佳佳, 金泓丞, 陈梦怡, 诸纪华. 4例心脏移植患儿的运动康复护理[J]. 中华护理杂志, 2026, 61(2): 249-253. |
| [14] | 徐晓佩, 李秋芳, 谈小雪, 吴玉洁. 1例妊娠合并李斯特菌感染致脓毒症休克并发噬血细胞综合征患者的护理[J]. 中华护理杂志, 2026, 61(2): 254-257. |
| [15] | 王雅雯, 孙菲, 秦钥, 沈绮怡, 雷霞, 周临. 丧失胎儿再次妊娠女性孕期体验与需求质性研究的Meta整合[J]. 中华护理杂志, 2026, 61(2): 258-266. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||