


中华护理杂志 ›› 2025, Vol. 60 ›› Issue (23): 2887-2894.DOI: 10.3761/j.issn.0254-1769.2025.23.010
杨范家一( ), 卫佳宁, 李晨霜, 孙长青, 刘延锦, 董小方(
), 卫佳宁, 李晨霜, 孙长青, 刘延锦, 董小方( )
)
收稿日期:2025-04-18
出版日期:2025-12-10
发布日期:2025-12-15
通讯作者:
董小方,E-mail:dongxiaofang1210@126.com作者简介:杨范家一:女,本科(硕士在读),E-mail:yangfanjiayi@163.com
基金资助:
YANG Fanjiayi( ), WEI Jianing, LI Chenshuang, SUN Changqing, LIU Yanjin, DONG Xiaofang(
), WEI Jianing, LI Chenshuang, SUN Changqing, LIU Yanjin, DONG Xiaofang( )
)
Received:2025-04-18
Online:2025-12-10
Published:2025-12-15
摘要:
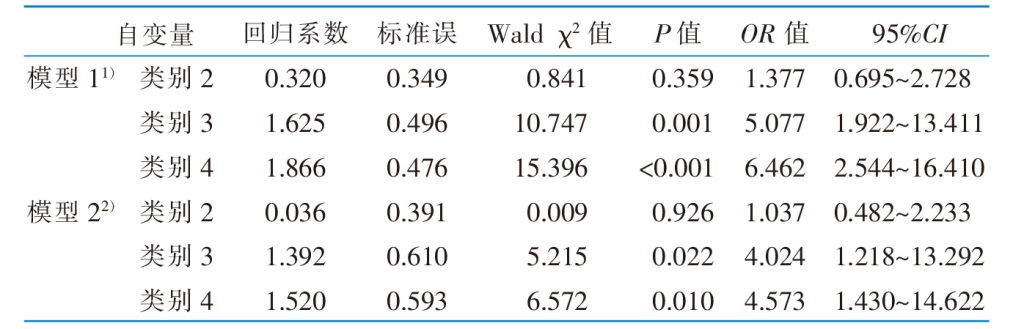
目的 探讨脑卒中患者客观睡眠质量轨迹及其与神经功能恢复之间的关系,为临床医护人员针对性开展睡眠干预提供依据。方法 采用多中心整群抽样方法,选取2023年11月—2024年7月河南省5所三级甲等医院神经内科362例脑卒中患者为调查对象,通过病历和问卷收集基线资料,三轴加速度计调查不同时间点睡眠质量,使用改良Rankin量表评估后遗症期神经功能恢复情况。采用并行潜类别增长模型识别睡眠质量轨迹,通过二元Logistic回归分析探讨不同轨迹对神经功能的影响。结果 共306例患者完成随访。睡眠质量轨迹分为睡眠质量持续良好组(34.31%)、短睡眠延长-效率升高-片段化改善组(49.02%)、长睡眠持续-效率降低-片段化加重组(7.84%)和睡眠质量持续不良组(8.83%)。多因素分析结果显示,工作状态、脑卒中类型、合并症、自理能力、社会支持、疲劳和抑郁是脑卒中患者睡眠质量轨迹的影响因素(P<0.05)。与睡眠质量持续良好组相比,长睡眠持续-效率降低-片段化加重组(OR=5.077)和睡眠质量持续不良组(OR=6.462)患者神经功能恢复不良的风险增加。结论 脑卒中患者睡眠质量轨迹存在异质性,不同轨迹对神经功能影响不同,医护人员应实施个性化睡眠管理以改善患者的神经功能。
杨范家一, 卫佳宁, 李晨霜, 孙长青, 刘延锦, 董小方. 脑卒中患者睡眠质量轨迹与神经功能恢复的关系研究及护理启示[J]. 中华护理杂志, 2025, 60(23): 2887-2894.
YANG Fanjiayi, WEI Jianing, LI Chenshuang, SUN Changqing, LIU Yanjin, DONG Xiaofang. Study on the relationship between sleep quality trajectories and neurological function recovery in stroke patients and its nursing implications[J]. Chinese Journal of Nursing, 2025, 60(23): 2887-2894.
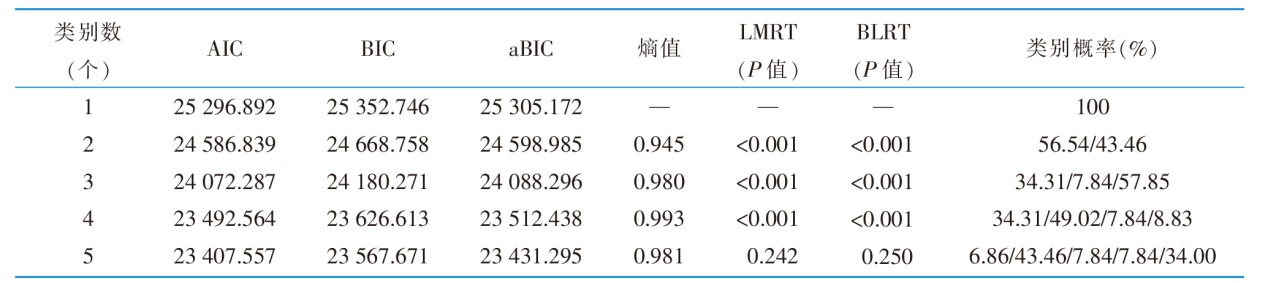 |
表2 脑卒中患者客观睡眠质量轨迹并行潜类别增长模型拟合指标(n=306)
Table 2 Objective sleep quality trajectory of stroke patients parallel latent class growth model fitting index(n=306)
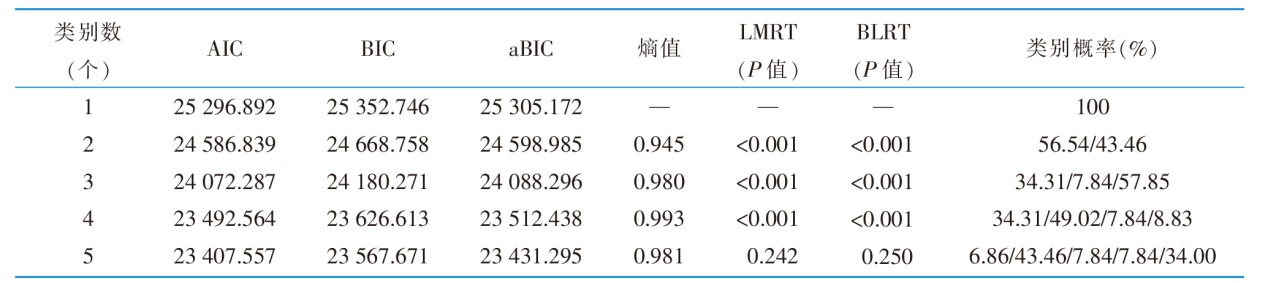 |
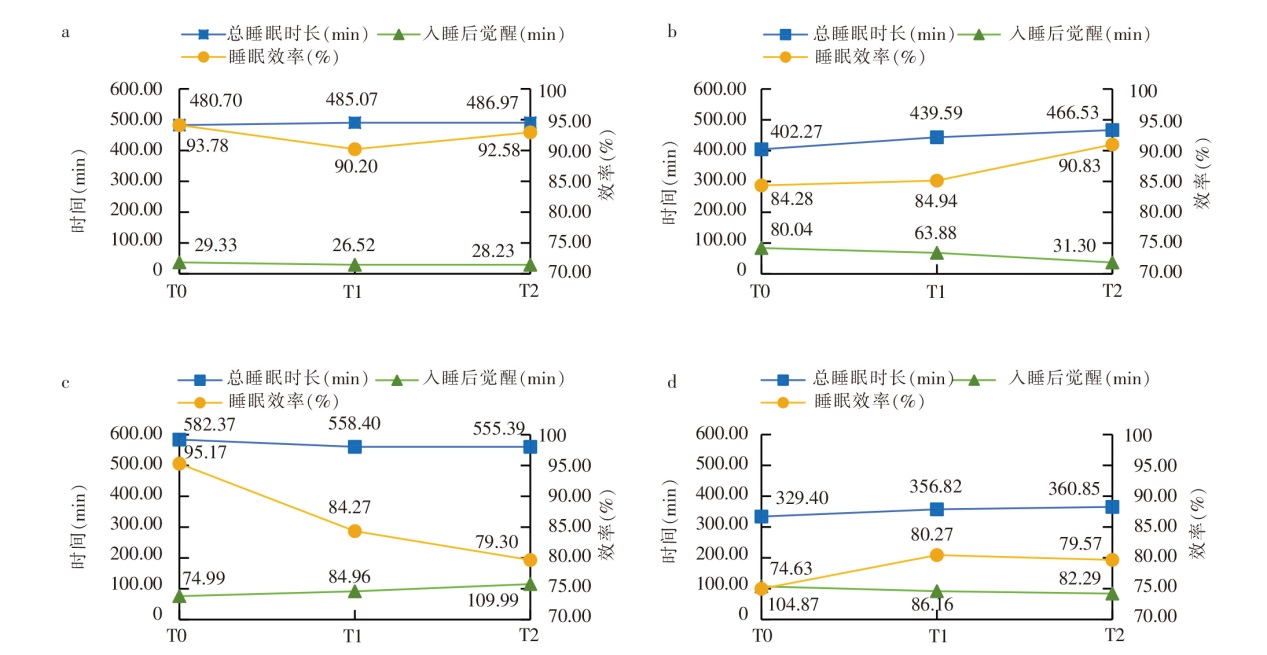
图1 脑卒中患者客观睡眠质量潜在类别发展轨迹 注:a为类别1:睡眠质量持续良好组。b为类别2:短睡眠延长-效率升高-片段化改善组。c为类别3:长睡眠持续-效率降低-片段化加重组。d为类别4:睡眠质量持续不良组。T0为发病1个月内,T1为发病后3个月,T2为发病后6个月。
Figure 1 The latent class development trajectory map of objective sleep quality in stroke patients
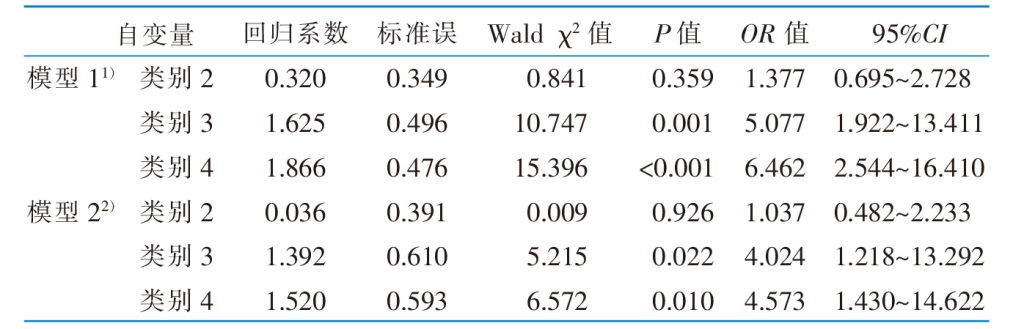 |
表5 脑卒中患者客观睡眠质量轨迹类别与神经功能恢复的二元Logistic回归分析(n=306)
Table 5 Binary logistic regression analysis of objective sleep quality trajectory and neurological recovery(n=306)
 |
| [1] | 中国脑卒中防治报告编写组. 《中国脑卒中防治报告2021》概要[J]. 中国脑血管病杂志, 2023, 20(11):783-793. |
| Report on Stroke Prevention and Treatment in China Writing Group. Brief report on stroke prevention and treatment in China,2021[J]. Chin J Cerebrovasc Dis, 2023, 20(11):783-793. | |
| [2] | Jeffers MS, Pittman AC, Kendzerska T, et al. Self-reported sleep disturbances among people who have had a stroke:a cross-sectional analysis[J]. CMAJ, 2023, 195(10):E354-E362. |
| [3] | Gottesman RF, Lutsey PL, Benveniste H, et al. Impact of sleep disorders and disturbed sleep on brain health:a scientific statement from the American heart association[J]. Stroke, 2024, 55(3):e61-e76. |
| [4] |
Schutte-Rodin S, Broch L, Buysse D, et al. Clinical guideline for the evaluation and management of chronic insomnia in adults[J]. J Clin Sleep Med, 2008, 4(5):487-504.
PMID |
| [5] |
Consensus Conference Panel, Watson NF, Badr MS, et al. Joint consensus statement of the American academy of sleep medicine and sleep research society on the recommended amount of sleep for a healthy adult:methodology and discussion[J]. J Clin Sleep Med, 2015, 11(8):931-952.
DOI URL |
| [6] | 中华医学会神经病学分会, 中华医学会神经病学分会脑血管病学组. 中国各类主要脑血管病诊断要点2019[J]. 中华神经科杂志, 2019, 52(9):710-715. |
| Chinese Society of Neurology,Chinese Medical Association; Cere-brovascular Diseases Study Group,Chinese Society of Neurology,Chinese Medical Association. Diagnostic criteria of major cerebrovascular diseases in China 2019[J]. Chin J Neurol, 2019, 52(9):710-715. | |
| [7] | 倪平, 陈京立, 刘娜. 护理研究中量性研究的样本量估计[J]. 中华护理杂志, 2010, 45(4):378-380. |
| Ni P, Chen JL, Liu N. The sample size estimation in quantitative nursing research[J]. Chin J Nurs, 2010, 45(4):378-380. | |
| [8] |
Kondrup J, Rasmussen HH, Hamberg O, et al. Nutritional risk screening(NRS 2002):a new method based on an analysis of controlled clinical trials[J]. Clin Nutr, 2003, 22(3):321-336.
DOI PMID |
| [9] |
Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies:development and validation[J]. J Chronic Dis, 1987, 40(5):373-383.
DOI PMID |
| [10] |
Kwah LK, Diong J. National Institutes of Health Stroke Scale(NIHSS)[J]. J Physiother, 2014, 60(1):61.
DOI URL |
| [11] |
Quinn TJ, Langhorne P, Stott DJ. Barthel index for stroke trials:development,properties,and application[J]. Stroke, 2011, 42(4):1146-1151.
DOI URL |
| [12] |
Cole RJ, Kripke DF, Gruen W, et al. Automatic sleep/wake identification from wrist activity[J]. Sleep, 1992, 15(5):461-469.
DOI PMID |
| [13] |
Podsiadlo D, Richardson S. The timed “up & go”:a test of basic functional mobility for frail elderly persons[J]. J Am Geriatr Soc, 1991, 39(2):142-148.
DOI PMID |
| [14] | 姜乾金. 领悟社会支持量表[J]. 中国行为医学科学, 2001, 10(10):41-43 |
| Jiang QJ. Perceived Social Support Scale[J]. Chin J Behav Med Sci, 2001, 10(10):41-43. | |
| [15] |
Dong XF, Liu YJ, Wang AX, et al. The psychometric properties of Chinese version of SCI Exercise Self-Efficacy Scale in patients with stroke[J]. Patient Prefer Adherence, 2016, 10:1235-1241.
DOI URL |
| [16] | 吴春薇, 王得新. 疲劳严重度量表中译本应用于脑梗死患者的临床与评价[J]. 中华物理医学与康复杂志, 2007, 29(9):608-611. |
| Wu CW, Wang DX. Clinical application and assessment of the Chinese version of Fatigue Severity Scale in stroke patients[J]. Chin J Phys Med Rehabil, 2007, 29(9):608-611. | |
| [17] | 何筱衍, 李春波, 钱洁, 等. 广泛性焦虑量表在综合性医院的信度和效度研究[J]. 上海精神医学, 2010, 22(4):200-203. |
| He XY, Li CB, Qian J, et al. Reliability and validity of a Generalized Anxiety Disorder Scale in general hospital outpatients[J]. Shanghai Arch Psychiatry, 2010, 22(4):200-203. | |
| [18] | 徐勇, 吴海苏, 徐一峰. 病人健康问卷抑郁量表(PHQ-9)在社区老年人群中的应用:信度与效度分析[J]. 上海精神医学, 2007, 19(5):257-259,276. |
| Xu Y, Wu HS, Xu YF. The reliability and validity of Patient Health Questionnaire Depression Module(PHQ-9) in Chinese elderly[J]. Shanghai Arch Psychiatry, 2007, 19(5):257-259, 276. | |
| [19] |
Banks JL, Marotta CA. Outcomes validity and reliability of the modified Rankin Scale:implications for stroke clinical trials:a literature review and synthesis[J]. Stroke, 2007, 38(3):1091-1096.
DOI URL |
| [20] | Zhou YY, Zheng H, Liang YM, et al. Joint developmental trajectories of bullying and victimization from childhood to adolescence:a parallel-process latent class growth analysis[J]. J Interpers Violence, 2022, 37(3/4):NP1759-NP1783. |
| [21] |
Ozkan H, Ambler G, Esmail T, et al. Prevalence,trajectory,and factors associated with patient-reported nonmotor outcomes after stroke:a systematic review and meta-analysis[J]. JAMA Netw Open, 2025, 8(2):e2457447.
DOI URL |
| [22] | 管士侠, 潘飞, 任韦宁, 等. 中青年缺血性脑卒中病人健康行为与睡眠质量的相关性研究[J]. 蚌埠医学院学报, 2021, 46(9):1316-1318. |
| Guan SX, Pan F, Ren WN, et al. Correlation between health behavior and sleep quality in young and middle-aged patients with ischemic stroke[J]. J Bengbu Med Coll, 2021, 46(9):1316-1318. | |
| [23] |
周柯冰, 黄晓娇, 闫凤侠. 首发脑卒中恢复期患者症状负担及其影响因素的网络分析[J]. 中华护理杂志, 2025, 60(7):792-798.
DOI |
|
Zhou KB, Huang XJ, Yan FX. Network analysis of symptom burden and its influencing factors in first-ever subacute stroke patients[J]. Chin J Nurs, 2025, 60(7):792-798.
DOI |
|
| [24] |
Guo LN, Zhang M, Namassevayam G, et al. Identification of sleep quality clusters among stroke patients:a multi-center latent profile analysis study[J]. Sleep Med, 2023, 112:203-208.
DOI URL |
| [25] |
邱雪斌, 繆小红, 夏敏棋, 等. 脑卒中患者疲劳轨迹的潜在类别及影响因素分析[J]. 中华护理杂志, 2024, 59(19):2375-2381.
DOI |
|
Qiu XB, Miao XH, Xia MQ, et al. Potential categories and influencing factors of fatigue trajectories in stroke patients[J]. Chin J Nurs, 2024, 59(19):2375-2381.
DOI |
|
| [26] |
Cabrera Y, Koymans KJ, Poe GR, et al. Overnight neuronal plasticity and adaptation to emotional distress[J]. Nat Rev Neurosci, 2024, 25(4):253-271.
DOI PMID |
| [27] |
Baranwal N, Yu PK, Siegel NS. Sleep physiology,pathophysiology,and sleep hygiene[J]. Prog Cardiovasc Dis, 2023, 77:59-69.
DOI PMID |
| [1] | 曾妃, 兰美娟, 顾培培, 梁江淑渊, 王衍蝶, 蔡凌云. 儿童双肺移植术后肺康复护理方案的构建及初步验证[J]. 中华护理杂志, 2025, 60(9): 1029-1035. |
| [2] | 阎寅至, 闻芳, 王敏, 周雪梅, 马金玲, 吴惠芳, 姚文英. 造血干细胞移植患儿运动康复分级护理方案的构建与应用研究[J]. 中华护理杂志, 2025, 60(9): 1036-1042. |
| [3] | 刘曦璇, 刘玉琳, 刘莎, 杨帆, 谢晓虹, 王紫娟, 刘丽芳, 魏红雨. 学龄期支气管哮喘患儿呼吸康复操的研制及效果评价[J]. 中华护理杂志, 2025, 60(9): 1043-1049. |
| [4] | 黄盼盼, 李丽玲, 胡晓静. 先天性心脏病婴儿早期运动康复的研究进展[J]. 中华护理杂志, 2025, 60(9): 1050-1055. |
| [5] | 陈丽鸥, 张文婷, 刘俊其, 王允琮, 王振霖, 齐赛, 杨娜. 肺叶体表投影定位结合肺段引流排痰技术对吸入性肺炎患者气道廓清的效果研究[J]. 中华护理杂志, 2025, 60(9): 1056-1061. |
| [6] | 杨娜娜, 程传丽, 曾慧, 符丹丹, 王燕, 陈悦, 冉宏敏, 范红静, 龙霞. 分级运动康复对慢性阻塞性肺疾病急性加重期患者的效果评价[J]. 中华护理杂志, 2025, 60(9): 1062-1067. |
| [7] | 曹云, 孙国珍, 陈凤, 季学丽, 闫梦婉, 敬雷, 钱堃. 改良式踝泵运动在脑卒中患者中的应用研究[J]. 中华护理杂志, 2025, 60(9): 1068-1074. |
| [8] | 谢敏, 漆文凯, 殷玲, 张旋, 赵如琴. 腹膜透析患者恐动症潜在剖面分析及影响因素研究[J]. 中华护理杂志, 2025, 60(9): 1080-1086. |
| [9] | 陈冰倩, 赵彬, 孙佳蓉, 郝四芳, 侯晓丽. 慢性牙周炎种植义齿患者口腔健康管理困境的质性研究[J]. 中华护理杂志, 2025, 60(9): 1087-1092. |
| [10] | 秦春兰, 吴振云, 钱红英, 赵茜, 孙锦庭. 慢性阻塞性肺疾病患者疾病自我控制体验的质性研究[J]. 中华护理杂志, 2025, 60(9): 1093-1098. |
| [11] | 李子崴, 冯丽娟, 陈旭升, 黄毅, 杨洁. PICC置管患者运动恐惧评估量表的编制及应用[J]. 中华护理杂志, 2025, 60(9): 1099-1106. |
| [12] | 程志强, 张宝珍, 汤利萍, 李静, 夏娇云, 魏雪岩, 龚智娴, 张美珍, 黎露思. 尿失禁患者疾病认知与态度量表的汉化及初步应用[J]. 中华护理杂志, 2025, 60(9): 1107-1112. |
| [13] | 杨静, 王华芬, 卢芳燕, 鲍瑞洁, 朱莉. 肝移植患儿术后营养状况变化的影响因素分析及护理启示[J]. 中华护理杂志, 2025, 60(9): 1113-1119. |
| [14] | 石美琴, 吴建芳, 张铎, 吴春萍, 陈玲, 陶磊. 1例全喉切除辅助发音管Ⅰ期植入患者术后喉功能康复的护理[J]. 中华护理杂志, 2025, 60(9): 1120-1123. |
| [15] | 谷茜, 黄玺, 施伟雄, 吴静, 谭若铭, 王枫. 1例T细胞免疫治疗后并发细胞因子释放综合征患者的护理[J]. 中华护理杂志, 2025, 60(9): 1124-1127. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||