


中华护理杂志 ›› 2024, Vol. 59 ›› Issue (19): 2396-2403.DOI: 10.3761/j.issn.0254-1769.2024.19.013
韩林( ), 李敏敏, 李雨欣, 陆柳伊, 张琦, 王雪婷, 鞠萍, 杨丽娟(
), 李敏敏, 李雨欣, 陆柳伊, 张琦, 王雪婷, 鞠萍, 杨丽娟( )
)
收稿日期:2024-01-28
出版日期:2024-10-10
发布日期:2024-10-14
通讯作者:
杨丽娟,E-mail:sdyanglijuan@aliyun.com作者简介:韩林:女,本科(硕士在读),护士,E-mail:710749736@qq.com
HAN Lin( ), LI Minmin, LI Yuxin, LU Liuyi, ZHANG Qi, WANG Xueting, JU Ping, YANG Lijuan(
), LI Minmin, LI Yuxin, LU Liuyi, ZHANG Qi, WANG Xueting, JU Ping, YANG Lijuan( )
)
Received:2024-01-28
Online:2024-10-10
Published:2024-10-14
摘要:
目的 构建先天性心脏病术后患儿营养不良风险预测模型,进行内部及外部验证。 方法 采用便利抽样法,选取2018年1月—2021年12月山东省某三级甲等医院收治的300例6月龄以下的先天性心脏病术后患儿作为建模组,选取2022年1月—2023年6月收治的129例患儿作为验证组。回顾性收集患儿的一般资料、疾病相关资料、治疗和护理相关资料,通过单因素、Logistic回归分析构建先天性心脏病术后患儿营养不良风险预测模型,绘制列线图并评价其预测效果。 结果 先天性心脏病术后患儿营养不良发生率为33.10%,Logistic回归分析结果显示,出生体重<2.5 kg、术前营养不良、术后1周液体负平衡、体外循环时间较长是患儿发生营养不良的危险因素(P<0.05)。该模型建模组受试者操作特征曲线下面积为0.933,灵敏度为83.30%,特异度为90.90%,Hosmer-Lemeshow检验显示,χ2=7.765(P=0.457)。验证组受试者操作特征曲线下面积为0.918,灵敏度为87.20%,特异度为90.00%,Hosmer-Lemeshow检验显示,χ2=4.947(P=0.763)。两组校准曲线均显示,该模型具有较好的校准度;临床决策曲线显示,该模型具有较好的临床实用性。 结论 该研究构建的风险预测模型具有较好的预测能力,可为医护人员早期识别先天性心脏病术后营养不良高危患儿,制订针对性干预措施提供参考。
韩林, 李敏敏, 李雨欣, 陆柳伊, 张琦, 王雪婷, 鞠萍, 杨丽娟. 先天性心脏病术后患儿营养不良风险预测模型的构建及验证研究[J]. 中华护理杂志, 2024, 59(19): 2396-2403.
HAN Lin, LI Minmin, LI Yuxin, LU Liuyi, ZHANG Qi, WANG Xueting, JU Ping, YANG Lijuan. Construction and verification of a risk prediction model for postoperative malnutrition in infants with congenital heart disease[J]. Chinese Journal of Nursing, 2024, 59(19): 2396-2403.
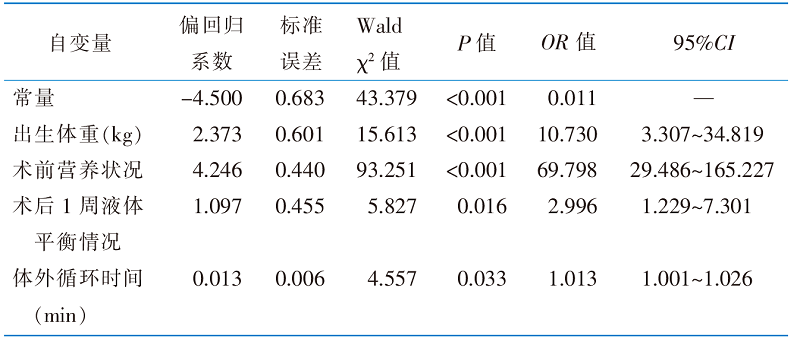 |
表3 先天性心脏病术后患儿营养不良的Logistic回归分析结果(n=300)
Table 3 Multivariate Logistic regression analysis of the influencing factors of postoperative malnutrition in children with CHD(n=300)
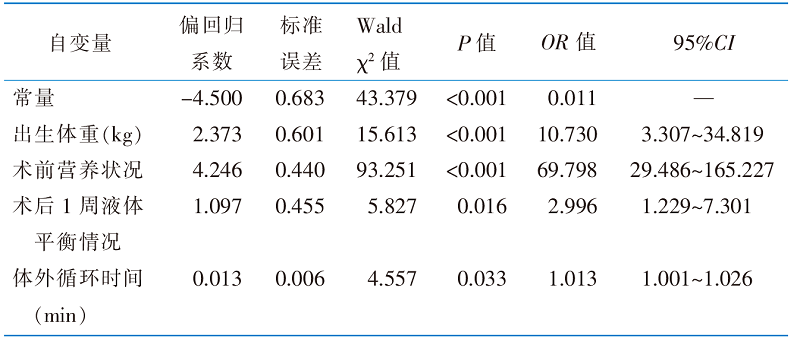 |
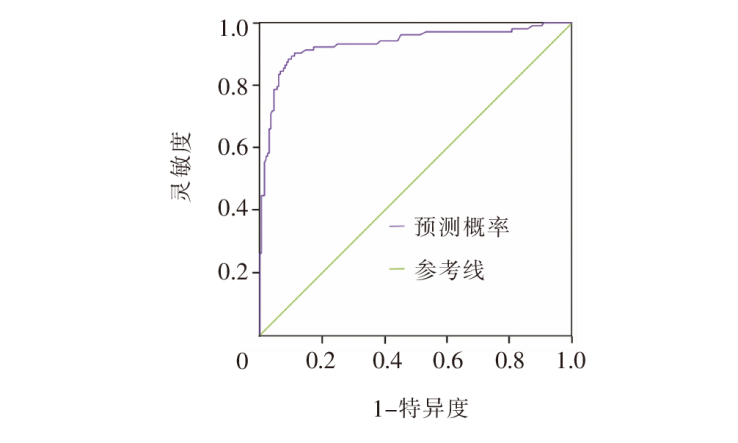
图2 建模组先天性心脏病术后患儿营养不良风险预测模型的受试者操作特征曲线
Figure 2 Receiver operating characteristic curve of the modeling group for predicting the risk of postoperative malnutrition in children with CHD
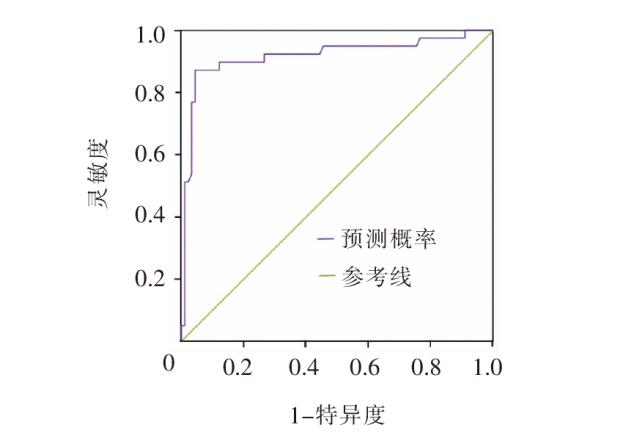
图3 验证组先天性心脏病术后患儿营养不良风险预测模型的受试者操作特征曲线
Figure 3 Receiver operating characteristic curve of the validation group for predicting the risk of postoperative malnutrition in children with CHD
| [1] |
傅唯佳, 顾莺, 杨玉霞, 等. 先天性心脏病患儿营养风险筛查及评估循证决策支持系统的构建与应用[J]. 中华护理杂志, 2023, 58(17):2059-2066.
DOI URL |
|
Fu WJ, Gu Y, Yang YX, et al. The construction and evaluation of an evidence-based decision support system for the nutrition risk screening of congenital heart disease children[J]. Chin J Nurs, 2023, 58(17):2059-2066.
DOI URL |
|
| [2] | Mehta NM, Corkins MR, Lyman B, et al. Defining pediatric malnutrition:a paradigm shift toward etiology-related definitions[J]. JPEN J Parenter Enteral Nutr, 2013, 37(4):460-481. |
| [3] | 张媛媛, 王海燕, 杨巧芳. 双重固定式约束衣在先天性心脏病患儿术后的应用[J]. 中华护理杂志, 2019, 54(1):137-139. |
| Zhang YY, Wang HY, Yang QF. The application effect of double fixed binding cloth in children with congenital heart disease surgery[J]. Chin J Nurs, 2019, 54(1):137-139. | |
| [4] | Martini S, Beghetti I, Annunziata M, et al. Enteral nutrition in term infants with congenital heart disease:knowledge gaps and future directions to improve clinical practice[J]. Nutrients, 2021, 13(3):932. |
| [5] |
Brief F, Guimber D, Baudelet JB, et al. Prevalence and associated factors of long-term growth failure in infants with congenital heart disease who underwent cardiac surgery before the age of one[J]. Pediatr Cardiol, 2022, 43(8):1681-1687.
DOI PMID |
| [6] | 顾晓蓉, 陈伟敏, 管咏梅. 6个月以下先天性心脏病患儿术后营养摄入状况的调查[J]. 解放军护理杂志, 2016, 33(12):49-50. |
| Gu XR, Chen WM, Guan YM. Investigation of postoperative nutrient intake of children with congenital heart disease aged under 6 months[J]. Nurs J Chin PLA, 2016, 33(12):49-50. | |
| [7] | Ross FJ, Radman M, Jacobs ML, et al. Associations between anthropometric indices and outcomes of congenital heart operations in infants and young children:an analysis of data from the Society of Thoracic Surgeons Database[J]. Am Heart J, 2020, 224:85-97. |
| [8] |
李莉娟, 胡春梅, 龚婷, 等. 先天性心脏病患儿术后1年营养不良影响因素分析[J]. 中华儿科杂志, 2023, 61(5):440-445.
PMID |
|
Li LJ, Hu CM, Gong T, et al. Factors associated with malnutrition in infants with congenital heart disease within one year after surgery[J]. Chin J Pediatr, 2023, 61(5):440-445.
DOI PMID |
|
| [9] |
Shi H, Yang D, Tang KC, et al. Explainable machine learning model for predicting the occurrence of postoperative malnutrition in children with congenital heart disease[J]. Clin Nutr, 2022, 41(1):202-210.
DOI PMID |
| [10] | 左茜, 苏洁, 陶柯宏, 等. 需体外循环手术干预的先天性心脏病婴幼儿的营养评估[J]. 心脏杂志, 2024, 36(2):191-195. |
| Zuo Q, Su J, Tao KH, et al. Nutritional assessment of infants with congenital heart disease requiring surgical intervention with extracorporeal circulation[J]. Chin Heart J, 2024, 36(2):191-195. | |
| [11] |
Centeno-Malfaz F, Moráis-López A, Caro-Barri A, et al. Nutrition in congenital heart disease:consensus document[J]. An Pediatr, 2023, 98(5):373-383.
DOI PMID |
| [12] | El-Chouli M, Meddis A, Christensen DM, et al. Lifetime risk of comorbidity in patients with simple congenital heart disease:a Danish nationwide study[J]. Eur Heart J, 2023, 44(9):741-748. |
| [13] |
Hansson L, Lind T, Wiklund U, et al. Fluid restriction negatively affects energy intake and growth in very low birthweight infants with haemodynamically significant patent ductus arteriosus[J]. Acta Paediatr, 2019, 108(11):1985-1992.
DOI |
| [14] |
高华炜, 陈求名, 赵韡, 等. 三种先天性心脏病手术风险评分系统预测效能的比较[J]. 中华心血管病杂志, 2019, 47(5):388-392.
PMID |
|
Gao HW, Chen QM, Zhao W, et al. Predictive value of 3 different risk stratification models for patients after congenital heart surgeries[J]. Chin J Cardiol, 2019, 47(5):388-392.
DOI PMID |
|
| [15] | 何洋, 李文星, 唐军, 等. 早产儿喂养不耐受临床诊疗指南(2020)[J]. 中国当代儿科杂志, 2020, 22(10):1047-1055. |
| He Y, Li WX, Tang J, et al. Clinical guidelines for the diagnosis and treatment of feeding intolerance in preterm infants(2020)[J]. Chin J Contemp Pediatr, 2020, 22(10):1047-1055. | |
| [16] |
Eveleens RD, Joosten KFM, et al. Definitions,predictors and outcomes of feeding intolerance in critically ill children:a systematic review[J]. Clin Nutr, 2020, 39(3):685-693.
DOI PMID |
| [17] | 丁文雯, 向奕瑾, 马佳莉, 等. 极低出生体重早产儿校正月龄12个月内体格生长情况及影响因素分析[J]. 中华护理杂志, 2019, 54(1):52-57. |
| Ding WW, Xiang YJ, Ma JL, et al. Analysis on features and related factors of physical growth in very low birth weight preterm infants in 12 months of corrected age[J]. Chin J Nurs, 2019, 54(1):52-57. | |
| [18] | 林淑皖, 张红, 涂惠琼. 母乳口腔运动干预对婴儿体外循环术后胃肠功能恢复的影响[J]. 护理学杂志, 2022, 37(21):36-39. |
| Lin SW, Zhang H, Tu HQ. Impact of olfactory stimulation with breast milk on digestive function recovery in infants after cardiopulmonary bypass[J]. J Nurs Sci, 2022, 37(21):36-39. | |
| [19] | Yilmaz Ferhatoglu S, Yurdakok O, Yurtseven N. Malnutrition on admission to the paediatric cardiac intensive care unit increases the risk of mortality and adverse outcomes following paediatric congenital heart surgery:a prospective cohort study[J]. Aust Crit Care, 2022, 35(5):550-556. |
| [20] | Wen BJ, Njunge JM, Bourdon C, et al. Systemic inflammation and metabolic disturbances underlie inpatient mortality among ill children with severe malnutrition[J]. Sci Adv, 2022, 8(7):eabj6779. |
| [21] |
Tsintoni A, Dimitriou G, Karatza AA. Nutrition of neonates with congenital heart disease:existing evidence,conflicts and concerns[J]. J Matern Fetal Neonatal Med, 2020, 33(14):2487-2492.
DOI PMID |
| [22] | 吴珍, 富智, 缪红军. 先天性心脏病新生儿围手术期营养支持的研究[J]. 肠外与肠内营养, 2017, 24(6):365-368,373. |
| Wu Z, Fu Z, Miu HJ. Nutrition support in neonates with congenital heart disease during the perioperative period[J]. Parenter Enter Nutr, 2017, 24(6):365-368,373. | |
| [23] |
Banerji N, Sudhakar A, Balachandran R, et al. Early weight trends after congenital heart surgery and their determinants[J]. Cardiol Young, 2020, 30(1):89-94.
DOI PMID |
| [24] | Hatami S, Hefler J, Freed DH. Inflammation and oxidative stress in the context of extracorporeal cardiac and pulmonary support[J]. Front Immunol, 2022, 13:831930. |
| [25] | Floh AA, McCrindle BW, Manlhiot C, et al. Feeding may modu-late the relationship between systemic inflammation,insulin resistance,and poor outcome following cardiopulmonary bypass for pediatric cardiac surgery[J]. JPEN J Parenter Enteral Nutr, 2020, 44(2):308-317. |
| [1] | 王龙君, 王丹, 徐海莉, 金歌, 方艳艳, 曾庆虎. 积木拼插游戏在学龄期PICC置管患儿上肢功能锻炼中的应用研究[J]. 中华护理杂志, 2024, 59(8): 947-952. |
| [2] | 韦双双, 游雪梅, 杨莉洁, 李繁荣, 唐如冰. 临终患儿父母哀伤辅导的证据总结[J]. 中华护理杂志, 2024, 59(5): 540-546. |
| [3] | 范晓睿, 顾莺, 胡静, 戚少丹, 贺琳晰, 张雯澜, 王林娟, 沈伟杰, 杨玉霞. 24所医院儿科ICU护士对患儿睡眠管理的认知及实践行为调查[J]. 中华护理杂志, 2024, 59(4): 447-454. |
| [4] | 孙潇潇, 陈朔晖, 滕燕萍, 王华, 刘丹. NICU早产儿的父亲出院准备度现状及影响因素分析[J]. 中华护理杂志, 2024, 59(4): 455-460. |
| [5] | 卢露, 卢芳燕, 吉莉, 陶玉侠, 姚彩萍. 6例小肠移植术后患儿肠造口的护理[J]. 中华护理杂志, 2024, 59(4): 461-464. |
| [6] | 鞠美涵, 李婷婷, 姜桐桐, 史铁英. 可治性先天畸形胎儿的母亲照顾准备度现状及影响因素分析[J]. 中华护理杂志, 2024, 59(20): 2495-2501. |
| [7] | 于万慧, 崔朝妹, 迟嘉婧, 靳子恒, 苟晓瑜, 李梦洁, 卢楠, 杨丽娟. 先天性心脏病青少年向成人过渡治疗及护理体验的Meta整合[J]. 中华护理杂志, 2024, 59(2): 219-227. |
| [8] | 李志茹, 卢芳燕, 吉莉, 戴燕红, 张婉莹, 王华芬. 护士主导的肝移植患儿腹内压管理方案的构建及应用研究[J]. 中华护理杂志, 2024, 59(19): 2319-2325. |
| [9] | 虞露艳, 周莹, 范佳杰, 吴倩, 褚小艺, 盛土君, 张稀, 白冠男, 林楠, 诸纪华. 肿瘤化疗患儿急性恶心呕吐非药物干预方案的构建及应用研究[J]. 中华护理杂志, 2024, 59(18): 2181-2188. |
| [10] | 范文琪, 赵蕊, 刘晓夏, 葛莉娜. 智能机器人在儿科患者疼痛干预中应用的范围综述[J]. 中华护理杂志, 2024, 59(18): 2277-2282. |
| [11] | 沙莎, 汤晓丽, 张莹, 秦嫣敏, 沈君怡, 金倩, 杨晓辰. 宫内环境模拟舱的设计及在早产儿中的应用[J]. 中华护理杂志, 2024, 59(18): 2300-2304. |
| [12] | 王康, 王俏, 李静. 虚拟现实技术在弱视患儿视觉训练中应用的范围综述[J]. 中华护理杂志, 2024, 59(16): 1948-1956. |
| [13] | 陈娅娟, 周蕊, 孙丹, 刘新文. 住院患儿静脉血栓栓塞症风险预测模型的构建及验证[J]. 中华护理杂志, 2024, 59(16): 1966-1972. |
| [14] | 易敏, 吴霞, 谭小艳, 钟丽娜, 杨琴, 陈艳萍, 刘花艳. 闭塞性细支气管炎患儿肺康复训练系统的研发与应用[J]. 中华护理杂志, 2024, 59(14): 1678-1686. |
| [15] | 何红梅, 喻芳, 林丽华, 舒芳. 急性胰腺炎患者再喂养综合征风险预测模型的构建及护理启示[J]. 中华护理杂志, 2024, 59(13): 1608-1615. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||