


中华护理杂志 ›› 2024, Vol. 59 ›› Issue (23): 2853-2859.DOI: 10.3761/j.issn.0254-1769.2024.23.006
王军( ), 卢舒颖, 纪媛媛(
), 卢舒颖, 纪媛媛( ), 王娜, 欧梦仙, 张娜芹, 崔丽, 李莉, 闫梦琦, 付思晨, 刘云云
), 王娜, 欧梦仙, 张娜芹, 崔丽, 李莉, 闫梦琦, 付思晨, 刘云云
收稿日期:2024-04-15
出版日期:2024-12-10
发布日期:2024-12-12
通讯作者:
纪媛媛,E-mail:jiyyuan@163.com作者简介:王军:女,硕士,主任护师,科护士长,E-mail:wangj229@126.com
基金资助:
WANG Jun( ), LU Shuying, JI Yuanyuan(
), LU Shuying, JI Yuanyuan( ), WANG Na, OU Mengxian, ZHANG Naqin, CUI Li, LI Li, YAN Mengqi, FU Sichen, LIU Yunyun
), WANG Na, OU Mengxian, ZHANG Naqin, CUI Li, LI Li, YAN Mengqi, FU Sichen, LIU Yunyun
Received:2024-04-15
Online:2024-12-10
Published:2024-12-12
摘要:
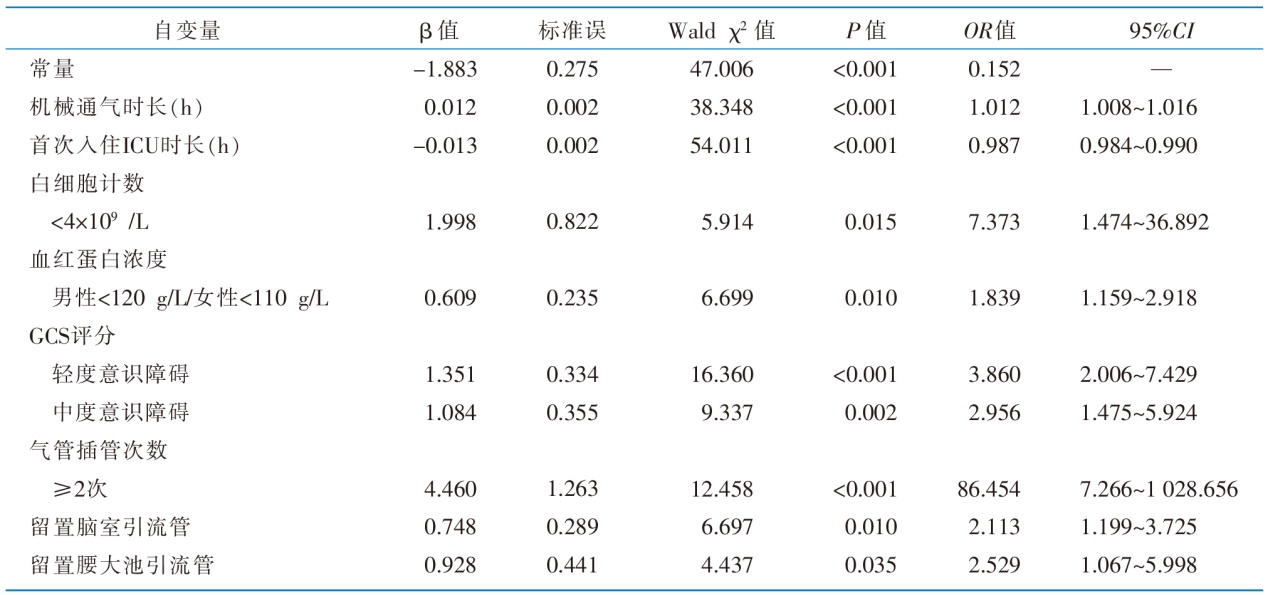
目的 了解神经外科患者非计划重返ICU发生现状及影响因素,旨在为临床医护人员制订有针对性的护理措施提供参考。方法 回顾性收集2020年1月—2022年9月北京市某三级甲等医院神经外科ICU转出患者的临床资料,使用倾向性评分匹配后得到组间协变量均衡的样本,并应用单因素和Logistic回归分析神经外科患者非计划重返ICU的影响因素。结果 共纳入4 789例患者资料,159例(3.32%)患者发生非计划重返ICU;以呼吸衰竭和肺部感染为主的呼吸系统并发症是造成神经外科患者非计划重返ICU的首要原因。Logistic回归分析显示,机械通气时长、首次入住ICU时长、气管插管次数≥2次、留置脑室引流管或腰大池引流管、转出ICU时存在轻中度意识障碍、白细胞计数低、血红蛋白计数低是神经外科患者非计划重返ICU的影响因素(P<0.05)。结论 医护人员应重视非计划重返ICU高风险人群,及时评估其转出风险,开展有针对性的护理措施并加强护理质量控制,以降低神经外科患者非计划重返ICU发生率。
王军, 卢舒颖, 纪媛媛, 王娜, 欧梦仙, 张娜芹, 崔丽, 李莉, 闫梦琦, 付思晨, 刘云云. 神经外科患者非计划重返ICU发生现状及影响因素研究[J]. 中华护理杂志, 2024, 59(23): 2853-2859.
WANG Jun, LU Shuying, JI Yuanyuan, WANG Na, OU Mengxian, ZHANG Naqin, CUI Li, LI Li, YAN Mengqi, FU Sichen, LIU Yunyun. Study on the current status and influencing factors of unplanned readmission to ICU for neurosurgical patients[J]. Chinese Journal of Nursing, 2024, 59(23): 2853-2859.
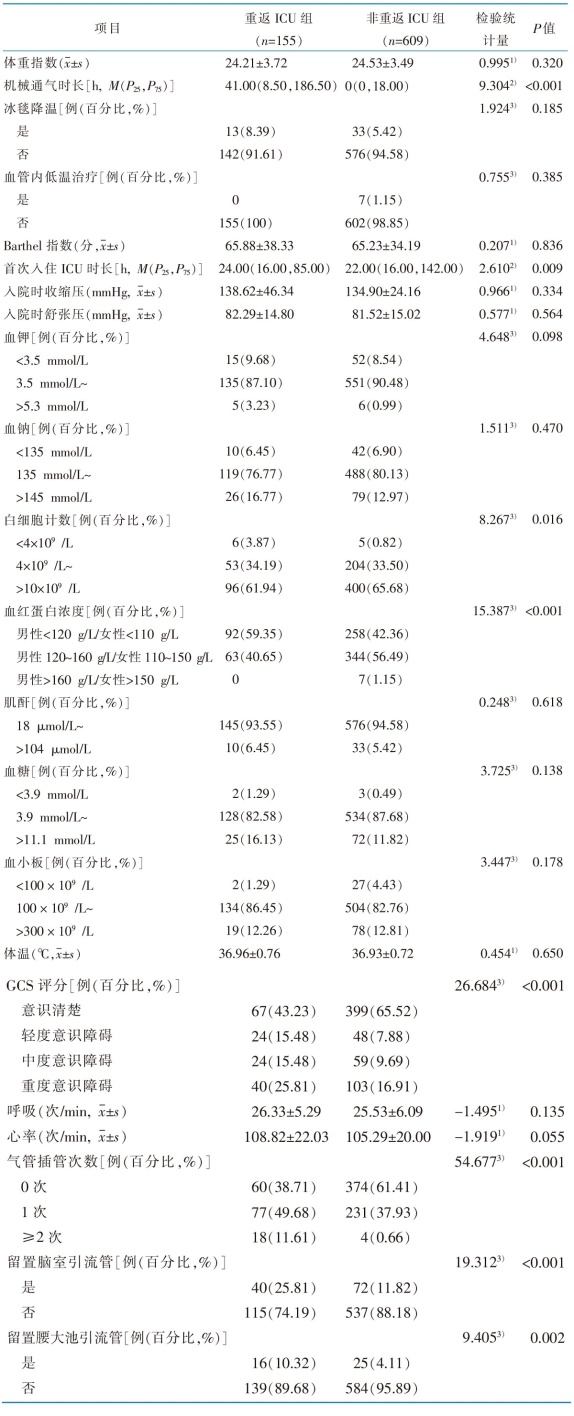 |
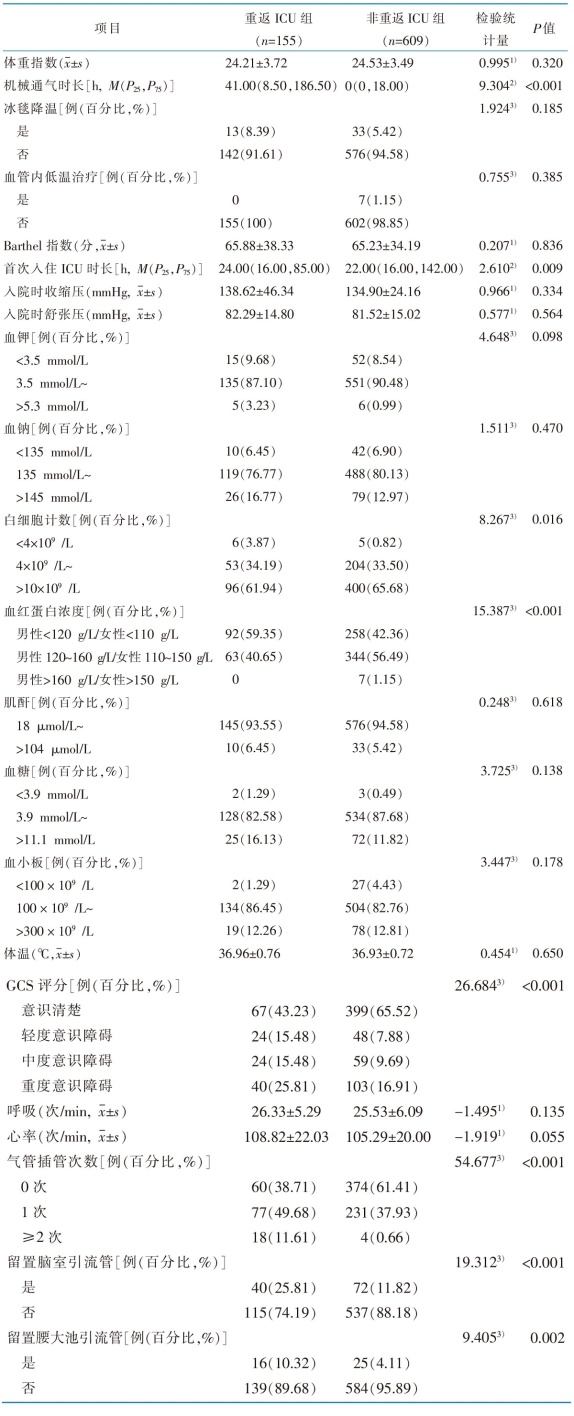
表2 倾向性评分匹配后神经外科患者非计划重返ICU影响因素的单因素分析
Table 2 Univariate analysis of influencing factors of unplanned readmission to ICU in neurosurgery patients after PSM
 |
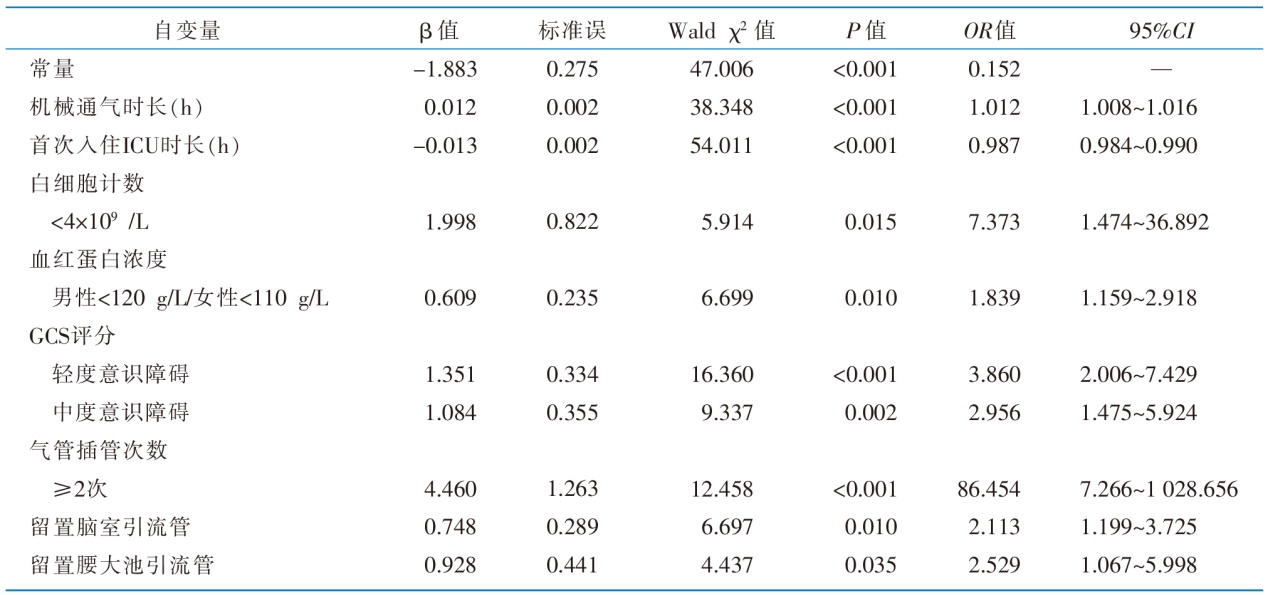 |
表3 倾向性评分匹配后神经外科患者非计划重返ICU影响因素的Logistic回归分析(n=764)
Table 3 Logistic regression analysis of influencing factors of analysis results of unplanned readmission to ICU in neurosurgery patients after PSM(n=764)
 |
| [1] | Yin YL, Sun MR, Zhang K, et al. Status and risk factors in patients requiring unplanned intensive care unit readmission within 48 hours:a retrospective propensity-matched study in China[J]. Risk Manag Healthc Policy, 2023,16:383-391. |
| [2] | AbuSara AK, Nazer LH, Hawari FI. ICU readmission of patients with cancer:incidence,risk factors and mortality[J]. J Crit Care, 2019,51:84-87. |
| [3] | Desautels T, Das R, Calvert J, et al. Prediction of early unplanned intensive care unit readmission in a UK tertiary care hospital:a cross-sectional machine learning approach[J]. BMJ Open, 2017, 7(9):e017199. |
| [4] | Nates JL, Nunnally M, Kleinpell R, et al. ICU admission,discharge,and triage guidelines:a framework to enhance clinical operations,development of institutional policies,and further research[J]. Crit Care Med, 2016, 44(8):1553-1602. |
| [5] | 胡佳民, 邹圣强, 江竹月, 等. 非计划重返ICU风险预测模型的构建与验证[J]. 中国护理管理, 2020, 20(4):519-524. |
| Hu JM, Zou SQ, Jiang ZY, et al. Development and verification of the risk predict model of unplanned readmission to comprehensive ICU[J]. Chin Nurs Manag, 2020, 20(4):519-524. | |
| [6] | 郝芳芳, 柳文娟, 林辉, 等. 肝胆胰术后患者非计划重返SICU的危险因素及预测模型[J]. 中华危重病急救医学, 2019(3):350-354. |
| Hao FF, Liu WJ, Lin H, et al. Readmission to surgical intensive care unit after hepatobiliary-pancreatic surgery:risk factors and prediction[J]. Chin Crit Care Med, 2019(3):350-354. | |
| [7] |
钱舒华, 朱新丽, 沈蓓蓓, 等. 孕早期和孕晚期焦虑状态对产妇分娩方式的影响[J]. 中华护理杂志, 2021, 56(2):245-249.
DOI URL |
|
Qian SH, Zhu XL, Shen BB, et al. Effects of anxiety about pregnant women in the first and third trimesters on the delivery modes[J]. Chin J Nurs, 2021, 56(2):245-249.
DOI URL |
|
| [8] | 孙颖浩, 贺佳. 临床研究设计及实践[M]. 北京: 人民卫生出版社, 2017. |
| Sun YH, He J. Clinical research design and practice[M]. Bei-jing: People’s Medical Publishing House, 2017. | |
| [9] | Mahoney FI, Barthel DW. Functional evaluation:the Barthel Index[J]. Md State Med J, 1965,14:61-65. |
| [10] | 侯东哲, 张颖, 巫嘉陵, 等. 中文版Barthel指数的信度与效度研究[J]. 临床荟萃, 2012, 27(3):219-221. |
| Hou DZ, Zhang Y, Wu JL, et al. Study on reliability and validity of Chinese version of Barthel Index[J]. Clin Focus, 2012, 27(3):219-221. | |
| [11] |
Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale[J]. Lancet, 1974, 2(7872):81-84.
DOI PMID |
| [12] |
Mayer SA, Dennis LJ, Peery S, et al. Quantification of lethargy in the neuro-ICU:the 60-second test[J]. Neurology, 2003, 61(4):543-545.
PMID |
| [13] |
黄丽红, 陈峰. 倾向性评分方法及其应用[J]. 中华预防医学杂志, 2019, 53(7):752-756.
PMID |
|
Huang LH, Chen F. The propensity score method and its application[J]. Chin J Prev Med, 2019, 53(7):752-756.
DOI PMID |
|
| [14] | 陈晓华, 陈俊宇, 王润东, 等. 行体外心肺复苏的院内心搏骤停患者使用主动脉内球囊反搏与住院死亡关系的研究[J]. 中华危重病急救医学, 2022, 34(3):269-273. |
| Chen XH, Chen JY, Wang RD, et al. Relationship of in-hospital mortality and using intra-aortic balloon pump with extracorporeal cardiopulmonary resuscitation in patients with cardiac arrest:a secondary analysis based on literature data[J]. Chin Crit Care Med, 2022, 34(3):269-273. | |
| [15] | Nathan CL, Stein L, George LJ, et al. Standardized transfer process for a neurointensive care unit and assessment of patient bounceback[J]. Neurocrit Care, 2022, 36(3):831-839. |
| [16] |
Lehmann F, Potthoff AL, Borger V, et al. Unplanned intensive care unit readmission after surgical treatment in patients with newly diagnosed glioblastoma-forfeiture of surgically achieved advantages?[J]. Neurosurg Rev, 2023, 46(1):30.
DOI PMID |
| [17] |
Tangonan R, Alvarado-Dyer R, Loggini A, et al. Frequency,risk factors,and outcomes of unplanned readmission to the neurological intensive care unit after spontaneous intracerebral hemorrhage[J]. Neurocrit Care, 2022, 37(2):390-398.
DOI PMID |
| [18] |
Park HS, Lee SH, Kim KM, et al. Readmission into intensive care unit in patients with aneurysmal subarachnoid hemorrhage[J]. J Cerebrovasc Endovasc Neurosurg, 2021, 23(4):327-333.
DOI PMID |
| [19] |
Coughlin DG, Kumar MA, Patel NN, et al. Preventing early bouncebacks to the neurointensive care unit:a retrospective analysis and quality improvement pilot[J]. Neurocrit Care, 2018, 28(2):175-183.
DOI PMID |
| [20] |
郭桂华, 许小明, 王海靓, 等. 脑卒中呼吸系统感染患者气道管理的最佳证据总结[J]. 中华护理杂志, 2023, 58(1):31-38.
DOI URL |
|
Guo GH, Xu XM, Wang HL, et al. Summary of the best evidence of airway nursing management in patients with respiratory infection after stroke[J]. Chin J Nurs, 2023, 58(1):31-38.
DOI URL |
|
| [21] | 周娥, 刘胤佃, 何金爱. 病人非计划重返监护室危险因素的Meta分析[J]. 循证护理, 2022, 8(8):1001-1008. |
| Zhou E, Liu YD, He JA. Risk factors for unplanned readmission to the ICU:a Meta-analysis[J]. Chin Evid-based Nurs, 2022, 8(8):1001-1008. | |
| [22] | 马淑娟, 程玮涛, 徐跃峤. 神经外科重症患者计划拔管失败的相关因素分析[J]. 神经损伤与功能重建, 2018, 13(4):184-186,189. |
| Ma SJ, Cheng WT, Xu YQ. Related factors of planned extubation failure in patients with severe brain injury[J]. Neural Inj Funct Reconstr, 2018, 13(4):184-186,189. | |
| [23] | Lee HW, Cho YJ. The impact of mechanical ventilation duration on the readmission to intensive care unit:a population-based observational study[J]. Tuberc Respir Dis, 2020, 83(4):303-311. |
| [24] |
黄彬彬, 王辉. 1例肺巨大肿瘤老年偏瘫患者术后肺复张的护理[J]. 中华护理杂志, 2024, 59(1):29-33.
DOI URL |
|
Huang BB, Wang H. Nursing care of postoperative lung re-expansion in an elderly hemiplegic patient with a massive pulmonary tumor[J]. Chin J Nurs, 2024, 59(1):29-33.
DOI URL |
|
| [25] | 余小燕, 厉春林, 张雅芝, 等. 脑室外引流管理的证据总结[J]. 中国护理管理, 2023, 23(11):1733-1737. |
| Yu XY, Li CL, Zhang YZ, et al. Evidence summary on external ventricular drain management[J]. Chin Nurs Manag, 2023, 23(11):1733-1737. | |
| [26] |
Cook AM, Morgan Jones G, Hawryluk GWJ, et al. Guidelines for the Acute Treatment of Cerebral Edema in Neurocritical Care Patients[J]. Neurocrit Care, 2020, 32(3):647-666.
DOI PMID |
| [27] | Belok SH, Bosch NA, Klings ES, et al. Evaluation of leukopenia during sepsis as a marker of sepsis-defining organ dysfunction[J]. PLoS One, 2021, 16(6):e0252206. |
| [28] | Travers S, Martin S, Litofsky NS. The effects of anaemia and transfusion on patients with traumatic brain injury:a review[J]. Brain Inj, 2016, 30(13/14):1525-1532. |
| [29] | Desjardins P, Turgeon AF, Tremblay MH, et al. Hemoglobin levels and transfusions in neurocritically ill patients:a systematic review of comparative studies[J]. Crit Care, 2012, 16(2):R54. |
| [30] | Liu GP, Zhao JT, Zeng Q, et al. Prevention and treatment of postoperative complication after clipping of intracranial aneu-rysm[J]. J Int Neurol Neurosurg, 2010, 37(6). |
| [1] | 韩冬芳, 田甜, 高畅, 张婧珺, 李小妹. 肺结核患者健康促进行为与健康心理控制源关系的混合研究[J]. 中华护理杂志, 2024, 59(9): 1029-1036. |
| [2] | 司茜茜, 王莹, 赵福云, 马晓骁, 刘均娥. A型主动脉夹层患者Ⅰ期心肺康复护理方案的构建及应用[J]. 中华护理杂志, 2024, 59(9): 1037-1042. |
| [3] | 沈支佳, 陈新宇, 钱志杰, 殷丽梅. 反复低血糖患者血糖管理行为退化特征的混合研究[J]. 中华护理杂志, 2024, 59(9): 1043-1050. |
| [4] | 王丽梅, 李露, 李玉霞, 喻鹏, 罗倩, 张翀旎. 糖尿病周围神经病理性疼痛患者运动恐惧现状及影响因素分析[J]. 中华护理杂志, 2024, 59(9): 1051-1056. |
| [5] | 丁慧敏, 戴莉敏, 蔡冬青, 杨群. 糖尿病前期患者自我管理潜在剖面分析及影响因素研究[J]. 中华护理杂志, 2024, 59(9): 1057-1064. |
| [6] | 刘海婷, 王咏梅, 郑贝贝, 蔡丽丽, 叶林斌, 吴佳芸, 宁丽, 李益民, 陈为霞. 冠心病合并糖尿病患者药物素养自评量表的编制及信效度检验[J]. 中华护理杂志, 2024, 59(9): 1065-1071. |
| [7] | 陈丽霞, 施慧, 朱德政, 曾莹. 成人低血糖恐惧评估工具的质量评价[J]. 中华护理杂志, 2024, 59(9): 1072-1079. |
| [8] | 中国研究型医院学会过敏医学专业委员会, 中华医学会变态反应分会过敏性疾病护理学组(筹), 中华预防医学会过敏病预防与控制专业委员会, (执笔:王青 刘君 支凡 万文锦 田丰英 霍晓鹏 周文华 杨永仕 王田田 孙劲旅). 变应原特异性免疫治疗皮下注射护理的专家共识[J]. 中华护理杂志, 2024, 59(9): 1080-1083. |
| [9] | 李琪, 苏晴晴, 张瑶瑶, 王田田, 吕静, 李亚可, 李海燕. 全膝关节置换患者关节遗忘变化轨迹及影响因素研究[J]. 中华护理杂志, 2024, 59(9): 1084-1090. |
| [10] | 刘娅, 刘晓晴, 杨雪凝, 王平, 刘学奎, 罗丹. 结肠镜检查患者肠道准备失败风险预测模型的构建及验证[J]. 中华护理杂志, 2024, 59(9): 1091-1098. |
| [11] | 孙晓晴, 张爱霞, 朱珠, 樊雪梅, 梅士娟, 黄欣欣, 丛胜楠, 谢红燕. 分娩心理创伤评估量表的编制及信效度检验[J]. 中华护理杂志, 2024, 59(9): 1099-1105. |
| [12] | 谢玉生, 黄蓉蓉, 赵雪, 马蕾, 胡雁, 杨倩, 王乾沙, 明玥. 成人重度烧伤患者肠内肠外营养的证据总结[J]. 中华护理杂志, 2024, 59(9): 1106-1113. |
| [13] | 李旭琴, 冯洁惠, 黄昉芳, 俞超, 梁诗雨, 王晓, 李旭芳, 朱含. 1例行机械循环辅助桥接心脏移植患者的术前护理[J]. 中华护理杂志, 2024, 59(9): 1114-1117. |
| [14] | 贾晓静, 陈一竹, 许志英, 和霞, 耿超. 1例尿黑酸尿症双膝关节置换术后患者并发急性心肌梗死的护理[J]. 中华护理杂志, 2024, 59(9): 1118-1121. |
| [15] | 顾培培, 曾妃, 兰美娟, 梁江淑渊, 郭璐瑶, 蔡凌云, 朱岩, 郭鸽. 肺移植患者衰弱影响因素的Meta分析[J]. 中华护理杂志, 2024, 59(9): 1122-1129. |
| 阅读次数 | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
全文 15
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
摘要 611
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||